Foot Problems
Are foot problems causing you pain and discomfort?
You’re not alone. Millions of people suffer from a variety of foot ailments, including athlete’s foot, corns, calluses, neuromas, stress fractures, warts, wounds, flat feet, and plantar fasciitis. These conditions can significantly impact your daily life, making it difficult to work, exercise, or simply enjoy your day.
At Hoyal Podiatry, we understand the frustration and pain associated with foot problems. Our team of experienced podiatrists is dedicated to providing comprehensive care and effective treatment solutions for a wide range of foot conditions. From diagnosing the root cause of your discomfort to developing a personalized treatment plan, we are committed to helping you regain foot health and mobility.
Athlete's Foot
Athlete’s foot is a common fungal infection that affects the skin of the feet, particularly between the toes. It is characterized by symptoms such as itching, burning, redness, and peeling skin. The infection is caused by fungi that thrive in warm and moist environments, such as sweaty shoes or public showers. Athlete’s foot is a common foot problem that can spread easily through contact with contaminated surfaces or by sharing personal items like towels or socks. Good hygiene, keeping feet clean and dry, and using antifungal treatments can help relieve symptoms and prevent the spread of the infection.
skin of the feet, particularly between the toes. It is characterized by symptoms such as itching, burning, redness, and peeling skin. The infection is caused by fungi that thrive in warm and moist environments, such as sweaty shoes or public showers. Athlete’s foot is a common foot problem that can spread easily through contact with contaminated surfaces or by sharing personal items like towels or socks. Good hygiene, keeping feet clean and dry, and using antifungal treatments can help relieve symptoms and prevent the spread of the infection.
Corn & Callus
A corn and callus are thickened areas of skin that form in response to repeated pressure or friction.
response to repeated pressure or friction.
A corn is a small, round, and hardened area of thickened skin that typically develops on the top or sides of the toes. It can be painful and may have a central core that presses into the deeper layers of the skin.
A callus, on the other hand, is a broader and larger area of thickened skin that commonly forms on the soles of the feet or the palms of the hands. It usually appears as a yellowish or grayish patch and may not cause pain unless it becomes excessively thick or cracked.
Both corns and calluses are not only a common foot problem but also the body’s way of protecting the skin from repeated rubbing or pressure. They can be caused by ill-fitting shoes, prolonged standing or walking, or certain foot deformities. While they are generally harmless, they can be bothersome or uncomfortable.
Treatment for corns and calluses typically involves reducing the pressure or friction on the affected area, such as wearing properly fitted shoes, using cushioning pads or inserts, or filing down the thickened skin with a pumice stone. In some cases, medical intervention may be necessary to remove the corn or callus.
Neuromas
Neuroma is a common but not well-know foot problem. A neuroma is a condition that involves the thickening of nerve tissue, most commonly occurring in the foot, between the metatarsal bones. It is often referred to as Morton’s neuroma. The thickening typically happens around the nerve that runs between the third and fourth toes.
tissue, most commonly occurring in the foot, between the metatarsal bones. It is often referred to as Morton’s neuroma. The thickening typically happens around the nerve that runs between the third and fourth toes.
Neuromas can cause pain, tingling, numbness, or a burning sensation in the ball of the foot or toes. Symptoms may worsen during walking or wearing tight shoes.
The exact cause of neuromas is not always clear, but factors such as wearing tight or high-heeled shoes, foot deformities, or repetitive stress on the feet can contribute to their development.
Treatment options for neuromas include wearing comfortable shoes with adequate toe space, using orthotic inserts for better foot support, applying ice packs to reduce inflammation, taking nonsteroidal anti-inflammatory drugs (NSAIDs) for pain relief, and in severe cases, corticosteroid injections or surgery may be recommended. Seeking medical advice is recommended for proper diagnosis and treatment.
Stress Fractures
A stress fracture is a small crack or hairline fracture that occurs in a bone. It is often caused by repetitive stress or overuse of the bone, commonly seen in athletes or individuals who engage in activities with high impact or repetitive movements.
occurs in a bone. It is often caused by repetitive stress or overuse of the bone, commonly seen in athletes or individuals who engage in activities with high impact or repetitive movements.
Unlike a complete fracture where the bone breaks entirely, a stress fracture involves a partial break that may not be immediately visible on an X-ray. The most common locations for stress fractures are the weight-bearing bones of the foot and lower leg, such as the metatarsals or shinbones.
Symptoms of a stress fracture may include pain that worsens with activity, swelling, tenderness, and sometimes bruising. Resting and avoiding activities that worsen the pain is essential for healing this foot problem.
Treatment for a stress fracture typically involves rest, immobilization with a cast or brace, and sometimes the use of crutches to reduce weight-bearing. In some cases, a physician may recommend nonsteroidal anti-inflammatory drugs (NSAIDs) for pain relief and physical therapy to aid in recovery.
Warts
Warts are small, rough growths that appear on the skin and are caused by a viral infection. They are typically non-cancerous and can occur on various parts of the body, such as the hands, feet, and face.
are caused by a viral infection. They are typically non-cancerous and can occur on various parts of the body, such as the hands, feet, and face.
Warts are caused by the human papillomavirus (HPV), which enters the skin through cuts or scratches. They are contagious and can spread through direct contact or by touching surfaces that have been in contact with the wart.
Warts, a common foot problem, can have different appearances depending on their type. Common warts are raised with a rough surface, often with black dots that are small blood vessels. Plantar warts occur on the soles of the feet and can be painful due to pressure. Flat warts are smaller and smoother, often appearing in clusters on the face, arms, or legs.
Most warts are harmless and can go away on their own over time. However, they can be bothersome or embarrassing, especially if they are in visible or sensitive areas.
Preventing the spread of warts involves avoiding direct contact with warts, keeping the skin clean and dry, not picking or scratching warts, and wearing footwear in public showers or swimming pool areas.
Wound Care/Ulcers
Wounds and ulcers are common foot problems among diabetics. Wound care and ulcers are open sores or wounds that occur on the feet. These wounds can result from various causes, such as diabetes, poor circulation, pressure, or injury. Podiatrists specialize in assessing and treating these wounds to promote healing and prevent complications. Wound care involves cleaning the wound, removing any dead tissue, and applying appropriate dressings or bandages to protect the area and promote healing. Podiatrists may also recommend offloading techniques to reduce pressure on the wound, such as padding or specialized footwear. In the case of diabetic foot ulcers, additional measures like infection management and blood sugar control may be necessary. Regular monitoring and follow-up visits are essential to ensure proper healing and prevent infection or further complications.
the feet. These wounds can result from various causes, such as diabetes, poor circulation, pressure, or injury. Podiatrists specialize in assessing and treating these wounds to promote healing and prevent complications. Wound care involves cleaning the wound, removing any dead tissue, and applying appropriate dressings or bandages to protect the area and promote healing. Podiatrists may also recommend offloading techniques to reduce pressure on the wound, such as padding or specialized footwear. In the case of diabetic foot ulcers, additional measures like infection management and blood sugar control may be necessary. Regular monitoring and follow-up visits are essential to ensure proper healing and prevent infection or further complications.
Flat Feet
Flat feet, also known as fallen arches, is a common foot problem in which 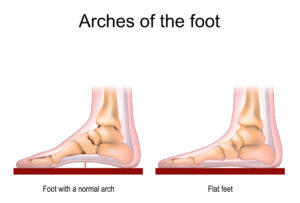 the arches on the inside of the feet are flattened, causing the entire sole of the foot to touch the ground when standing.
the arches on the inside of the feet are flattened, causing the entire sole of the foot to touch the ground when standing.
Normally, the arches in the feet help distribute body weight evenly and provide shock absorption. However, in individuals with flat feet, the arches are lower or completely absent, which can lead to various symptoms.
People with flat feet may experience pain or discomfort in the feet, ankles, or lower legs. They may also have an inward rolling motion of the foot (overpronation) while walking or running, which can affect their gait and potentially lead to other issues such as knee or hip pain.
Treatment for flat feet typically involves managing symptoms through supportive measures. This may include wearing supportive shoes with arch support or custom orthotic inserts to provide stability and relieve discomfort. Physical therapy exercises can also help strengthen the muscles in the feet and legs. In some cases, medical intervention such as braces or surgery may be recommended.
Plantar Fasciitis
Plantar fasciitis is a common foot problem characterized by pain in the heel or bottom of the foot. It occurs when the plantar fascia, a thick band of tissue that connects the heel bone to the toes, becomes inflamed or irritated.
pain in the heel or bottom of the foot. It occurs when the plantar fascia, a thick band of tissue that connects the heel bone to the toes, becomes inflamed or irritated.
The plantar fascia acts like a shock-absorbing bowstring, supporting the arch of the foot. However, repetitive strain or overuse can cause tiny tears in the fascia, leading to pain and discomfort.
People with plantar fasciitis often experience sharp or stabbing pain in the heel, especially in the morning or after periods of rest. The pain may improve with movement but can worsen after long periods of standing or walking.
Several factors can contribute to plantar fasciitis, including high-impact activities, inadequate footwear, obesity, and foot mechanics such as flat feet or high arches.
Treatment for plantar fasciitis typically involves conservative measures. These may include rest and avoiding activities that worsen the pain, applying ice to reduce inflammation, stretching exercises to stretch the calf and plantar fascia, wearing supportive shoes or orthotic inserts for better arch support, and taking over-the-counter pain medications. Physical therapy, night splints, and corticosteroid injections may also be recommended in some cases.
In most instances, plantar fasciitis can be managed effectively with these measures.